Hyaluronic Acid Injections
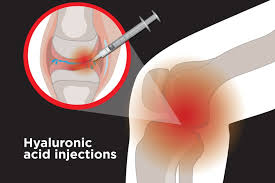
Hyaluronic acid injections (also known as viscosupplements) are used to treat osteoarthritis of the knee and other joints.
Osteoarthritis occurs when the cartilage in your joint that cushions the ends of the bones gradually wears down. Cartilage aids in frictionless joint motion. When the cartilage wears down completely, the joints are left vulnerable to wear and tear. When this happens, it causes your bones to rub together, resulting in pain, joint stiffness and swelling.
Injecting the affected area with hyaluronic acid injections aids in protecting, cushioning, and lubricating the joints.
This type of injection may be effective to reduce pain and improve function for up to 6 months.
Intraarticular Corticosteroid (Steroid) Injections
Steroid injections are often recommended for people with rheumatoid arthritis and other types of inflammatory arthritis. They may also be recommended for osteoarthritis if your joints are very painful or if you need extra pain relief for a time. The injection can reduce inflammation, which in turn should reduce pain.
Steroid injections can’t treat the underlying cause of your condition, but they can treat the symptoms.
A number of different steroids are available for injection.
Some steroid injections start to relieve pain within hours and the effects should last about a week. Your doctor or other healthcare professional might call these short-acting soluble steroids. Soluble means that the drug dissolves quickly in your body and starts working quickly.
Other steroid injections take around a week to become effective but can ease your symptoms for two months or longer. These are described as less soluble because the drug takes longer to get into your system.
Due to of significant health risks, frequent injections of steroids are not recommended.
Epidural Injection Of Corticosteroids (Cortisone)
Epidural injection delivers a mixture of medications into the space around your spinal cord or nerve roots (epidural space). An epidural injection is a way to achieve a high concentration of anti-inflammatory medication (cortisone) at the site of a herniated disc, or narrowed spinal canal (spinal stenosis) . The injections work the best for a nerve pain in leg (sciatica) or arm. They are not indicated for treatment of back pain.
Nerve Blocks
Pain in your back and/or neck (or occipital headaches) can come from the facet joints in your spine. To determine if this is the reason you are having pain and to consider more lasting therapy, we first have to perform diagnostic tests by “blocking” or numbing the nerves that supply those joints with local anesthetic. This is usually done twice to compare results.
As this is only a test, it is meant to be temporary. Depending on the results, you may be recommended another procedure called radiofrequency neurotomy that “burns” these tiny nerves to those painful joints. This again is safe as it is done nearly the same way as the test but offers more long-lasting results.
What to expect during the diagnostic facet block tests:
You will be awake during these tests so that you can assess whether your pain has changed or not. While lying on your stomach, small needles are placed carefully and precisely near the tiny nerves for the facet joints using x-ray control for accuracy and safety. Usually 4-8 injection sites are required. The needles are outside of the spinal cord, therefore no damage to the spinal cord can occur. As with most procedures, there is a risk of tenderness, bleeding and/or bruising at the injection sites, and very rarely infection, nerve damage, allergy or seizure. Sometimes steroid is also used for possible therapeutic value, which can uncommonly cause high blood sugar or blood pressure, transient flushing water retention, swelling, and rare ulcers, cataracts, or hip arthritis (AVN).
Neuromuscular Electrical Simulation (NMES)
Spinal pain is multifactorial. Pain can be initiated by some combination of overuse, muscle strain, and/or injuries to the muscles, ligaments, joints and discs that support the spine. Over time, a muscle injury that has not been managed correctly may lead to atrophy (waste). This can lead to constant discomfort and/or pain causing the affected person to limit their activity even further. Eventually, protective mechanisms fail, and a fear of re-injury remains (kinesiophobia). Therefore, regardless of the initial event the main goal is to reactivate the muscles and restore normal function. Because each problem is treated with different protocols, it is important to consult with a medical professional before beginning any strenuous rehabilitation program.
Exercise and flexibility can be the best treatment option for almost all types of musculoskeletal problems as it is likely to help restore balance in the spine. Exercise focused on strengthening of the abdominal and paraspinal muscles, leading to stabilization of the spine. Rehabilitation programs or preventative rehabilitation programs that focus on conditioning, combined with core stability and proprioception (position sense) will reduce the risk of pain if exercises are done correctly, and on a regular basis. Restorative yoga or pilates are especially effective to rebuild stamina and reactivation of core muscles. Deeper muscles’ (multifidus) activation is mostly subconscious. Over time, patients learn how to activate those muscles.
A faster way that may be initially used is to electrically stimulate the muscle by either non-invasive or invasive (needle) methods. Neuromuscular electrical muscle stimulation (NEMS) can be done using a TENS-type device with a non-fatigue muscle activation mode. In case an invasive option is necessary EMG-type needle is placed under ultrasound guidance and the stimulation is initiated. Usually 10-12 sessions with concomitant physiotherapy are necessary to achieve clinical results.
